Does heat affect diabetes is a question we have been asking now that summer is just a few weeks away?
We have learned through our grandson’s journey with Type 1 Diabetes that with careful planning and proper blood glucose management diabetics can participate in many of the same activities the rest of us can regardless of the season.
The summer heat affects many people in different ways. I love the heat and tend to spend as much time as possible outdoors in my gardens. My husband on the other hand finds the heat difficult to work in, the heat just saps his energy.
It was these very different reactions to the same temperature that got me wondering how the heat may affect a diabetic or more specifically, our grandson.
We wanted to know what to expect or what to look out for to ensure his safety.
Table of Contents
How the Heat May Affect You
For a person with diabetes, they may find it harder for their body to handle high heat and humidity. Once temperatures reach 27°C (about 80°F) or higher, especially in humidity, it can have a significant effect on diabetes medications, testing supplies, and your health.
The extreme heat of summer will definitely affect your blood glucose levels.
Just what that effect depends on what you have eaten, your level of hydration, and activity level.
If you are getting quite sweaty between the heat and your activity, you may become dehydrated which will cause your blood glucose levels to rise. This can create a vicious cycle because:
- dehydration will make your blood glucose levels rise
- this makes you thirsty so you drink more
- which makes you urinate more
- which further dehydrates you
- dehydration reduces blood supply to the skin which means less of the injected insulin will be absorbed by the body
As you can see it creates quite a dangerous cycle. Try to prevent dehydration by increasing the amount of water you drink through the hot summer months.
How the Heat May Affect Test Equipment or Medications
Diabetes medications, glucose meter, and diabetes test strips can be affected by high summer temperatures.
Insulin and other medications can quickly become degraded and ineffective.
For this reason, it is imperative to properly store your medications away from the extreme heat. For instance, never leave them in a sweltering car.
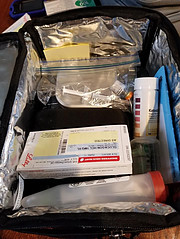
If you are traveling or will be out for the day taking your medications in a cooler is a great idea. Make sure your medications are not directly on the ice pack as the direct cold will affect them as well.
Adjusting Insulin Dosage
The majority of today’s insulin can easily tolerate temperatures in the 33 – 35 degrees C (93 – 95 degrees F) range but they will rapidly degrade with temperatures higher than that. Carry insulin in an insulated bag preferably with a pocket for an ice pack.
If you are physically active you may require less insulin. This may increase your risk of low blood sugars making it necessary to also take along some fast-acting sugar snacks to treat lows.
Be sure to test glucose and make any necessary adjustments before physical activity.
Work closely with your health care team to determine the best treatment plan for you.
Be sure to tell your doctor if things are not working for you so he can help make any dosage adjustments.
Tips for Managing Blood Glucose
Just because it is hot outside doesn’t mean you need to be confined indoors. With a few precautions, you enjoy the great outdoors all summer long.
These tips will help ensure an enjoyable summer outdoors:
- Drink plenty of water. Carry waters with you to make it easier to stay hydrated. If you will be engaging in a heavy activity it would be a good idea to also have a sports drink to replace electrolytes as well.
- Adjust insulin as necessary. Your doctor will advise you on how you should adjust your insulin before exercising. Be sure to tell your doctor what type of exercise you will be engaging in and for how long of a period.
- Test your blood sugars frequently. Hot weather can make your levels fluctuate more than usual so testing more frequently is advised. Test often for several hours after physical activities as these can affect you for a longer period.
- Have treatments for Lows with you. This could be glucose tabs or gel. It is also a good idea to have a glucagon kit with you just in case of a severe low.
- Take a snack. Some snacks may serve as a meal replacement while other snacks may be used to treat mild lows. Your nutritionist can help you come up with great options.
- Protect medications and supplies. Take medications, supplies, snacks, and water in an insulated cooler. Ensure the medications and test kits are not directly on the ice or cold pack. Insulin pumps and continuous glucose monitors should be OK in the heat just don’t expose them to direct sun for very long.
- Avoid sunburn. Regardless of the activity, it is always possible to get sunburn so be sure to wear a broad-spectrum sunscreen and wear protective eyewear and a hat. Sunburn can stress the body which can raise blood sugar levels.
Finally
Summer will soon be upon us and understanding just how does heat affect diabetes is important to fully enjoy this wonderful season.
A few simple precautions can help you have a safe, fun, and active summer despite the extreme heat.
Exercise is an important part of diabetes management but try not to be outside at the hottest time of the day. Try to be active in the cooler times, early morning, or evening.
Always wear shoes and be diligent about checking your feet each day.
Test your glucose levels more often and know the signs of low blood sugar, They can be easily confused with heat exhaustion so be sure to test your blood sugars.
Store your medications and your supplies away from extreme heat.
Keep in mind that perspiration can loosen the adhesives on continuous glucose monitors (CGM’s) and insulin pumps. Your sensor or infusion set may loosen. Check them often and talk with your diabetes care team if this is a problem. They may have suggestions to help.
Try to keep as cool as possible while enjoying the great outdoors as much as possible.
Thanks for dropping by. Feel free to share your summer tips in the comment section below. I look forward to learning your tips for summer.


Thank you for this article.
I really did not know that there was an effect between heat and diabetes.
I like that you also provided tips that can be helpful in this manner such as drinking more water and avoiding sun burn.
As I am discovering with our grandson, there are seemingly normal everyday things that can profoundly affect his blood glucose levels. When it comes to the health and safety of our diabetic friends and family members, education is the key. Avoiding sunburn and drinking plenty of water on hot summer days is important for everybody not just diabetics although it is more important for them. Thanks for reaching out.